Consistent stomach ache? Battling a bloated gut all too often? Diarrhea affecting daily life? Celiac disease could be the cause. An estimated 2 million people in the U.S. live with this chronic digestive and immune disorder, according to the National Institute of Diabetes and Digestive and Kidney Diseases.
The protein gluten, which can be found in grains like wheat, is what causes celiac disease. The disease sparks an autoimmune response, causing the body to attack nutrient-absorbing structures in the small intestine called villi. In the absence of treatment, this damage may contribute to the following conditions:
- Anemia (low red blood cells)
- Fertility issues in women of childbearing age
- Nutritional deficiencies
- Osteoporosis (bone weakness)
- Cancer of the small intestine
Adopting a gluten-free lifestyle can be an easy and effective treatment for some people with celiac disease. As with any change in routine, going gluten free can be an adjustment, but learning something new is usually well worth the effort when it comes to feeling better. Note that not everyone who goes gluten-free is relieved of all symptoms.
Know the symptoms of celiac disease
Celiac disease can develop at any age and symptoms can differ from person to person. In general, some common signs to look for include regular bouts of:
- Abdominal pain
- Bloating
- Constipation
- Diarrhea
Unexpectedly reduced weight Lesser-known celiac disease symptoms can include:
- Brain fog
- Dermatitis herpetiformis—an itchy vascular rash
- Fatigue
- Mental health changes
On rare occasions, a person may have celiac disease without symptoms. This phenomenon is called silent celiac. It is typically discovered when routine laboratory tests reveal vitamin deficiencies that cannot be explained. Symptoms may eventually appear as the body continues to attack the small intestine.
Talk about the diagnosis with your doctor
Talk to your doctor about any GI concerns you may have because celiac disease presents in a variety of ways. And be sure to discuss symptoms before cutting gluten out of your diet. This ensures that any suggested diagnostic blood test will be as accurate as possible.
In addition to assessing symptoms, your doctor can talk with you about family history and genetics that could play a role. For instance, individuals who have celiac disease in a parent, sibling, or even child may be at greater risk. Also, those with a wheat-heavy heritage—such as those from the the global “Wheat Belt” or with an Italian lineage—may be more susceptible to celiac disease.
A straightforward blood test to check for antibodies in the blood that indicate a reaction to gluten is the first step if diagnostic testing is the way to go. The presence of these antibodies could suggest celiac.
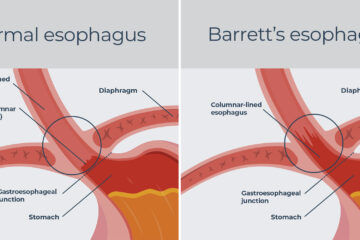
The second step is an upper endoscopy. During this safe outpatient procedure, a gastroenterologist slides a slender tube down your throat to take a look at the small intestine. They’ll examine tissue lining the small intestine and take a tiny sample to test for damage.
Gluten sensitivity and celiac disease are different
Your symptoms may be caused by a wheat allergy or gluten sensitivity if tests rule out celiac disease. If this is the case, doctors might suggest a gluten challenge, which involves keeping track of your symptoms and watching how much gluten you eat to see if there is a connection.
Although they do not cause damage to the small intestine, gluten intolerance, allergies, or sensitivities share many of the same signs and symptoms as celiac disease. The primary distinction between celiac disease and gluten reactions is the injury component.
A gluten-free diet can help manage celiac disease
If you have been diagnosed with celiac disease, it is time to alter your diet. A gluten-free diet can successfully manage celiac disease, but there is currently no medication to treat the condition. When there is no gluten in the body, there is no harmful gut reaction and no recurrence of symptoms.
Some common gluten-heavy foods to avoid are:
- Bread
- Cake
- Crackers
- Pasta
- Soup
Understanding how to approach a gluten-free diet isn’t something you need to figure out on your own; a registered dietitian can help you tailor a plan that’s works with your life.
Gluten-free food options in grocery stores and restaurants are expanding in tandem with the rise in celiac disease awareness. This empowers patients to continue enjoying foods and the socialization of going out to eat. But, of course, there’s always a risk of cross contamination, especially at a restaurant. We often advise patients to consider cooking at home while getting used to gluten-free eating.
Keep in mind that some supplements and vitamins, for example, may contain gluten as an ingredient. To help ingest as little gluten as possible, patients can tap into resources like the National Library of Medicine’s database to identify medications with gluten.
We typically re-test for gluten antibodies after three to six months of following a gluten-free diet. Those antibodies usually disappear around six months if a gluten-free lifestyle is in place, which means the small intestine is no longer being injured and symptoms are likely under control.
Talk with your doctor about symptoms
If you suspect celiac disease is the culprit of unpleasant gut problems, speak with your doctor right away.
Keep in mind that if you’ve been diagnosed with celiac disease, you’re not alone. Your family and friends, primary care provider, gastroenterologist, and nutritionist can provide holistic support along your gluten-free journey.