Women’s health is not a single chapter—it’s a lifelong journey that spans adolescence, reproductive years, mental health, pregnancy, menopause, and beyond. Because these stages often involve different clinicians, specialties, and care priorities, maintaining continuity over time can be difficult.
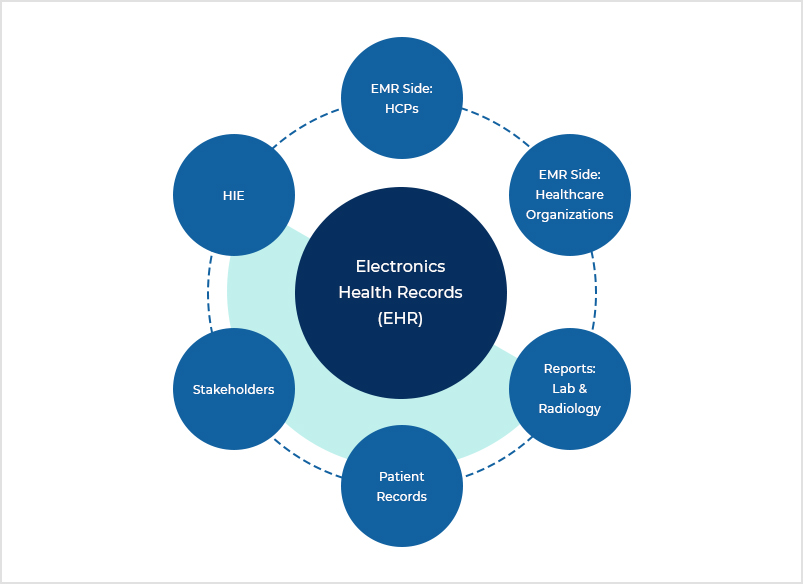
As women’s healthcare evolves, electronic health record (EHR) systems are increasingly expected to do more than document individual visits. Today, they are designed to support long-term continuity, care coordination, and clinical insight across every phase of a woman’s life. When implemented effectively, an EHR becomes the foundation of comprehensive women’s healthcare—connecting clinicians, preserving medical history, and supporting better outcomes.
Modern EHRs also help women’s health organizations navigate complex billing structures and contribute de-identified data that advances research into health trends, outcomes, and disparities. Here’s how EHR systems are strengthening care across the full spectrum of women’s health.
Preserving a complete medical history across life stages
Women’s healthcare often spans multiple specialties, from primary care and obstetrics to cardiology, endocrinology, and menopause management. Without a centralized system, critical information can easily become scattered across disconnected records.
A modern EHR brings this information together in one place. Clinicians can document and link key health events such as menstrual and contraceptive history, pregnancies and births, postpartum care, surgeries, mental health conditions, and chronic illnesses. This unified record gives providers valuable context for clinical decisions and supports preventive care and early intervention.
When clinicians can quickly access a woman’s full medical history, they’re better equipped to make informed decisions and avoid unnecessary repeat tests or treatments. Many EHR platforms now enhance this process with advanced data capture and decision-support tools, including AI-powered features that improve documentation quality and streamline workflows.
Improving care coordination across providers and specialties
Fragmented care remains a common challenge. A woman may see a primary care provider for diabetes, an Ob-Gyn for prenatal care, and later a specialist for postpartum hypertension or cardiovascular concerns. When these providers work in separate systems, communication gaps can delay care or lead to duplication—such as repeated lab tests or conflicting treatment plans.
A robust EHR reduces these risks by giving all authorized clinicians access to up-to-date information, including medications, allergies, test results, and care plans. Shared documentation supports smoother referrals, consistent patient communication, and safer transitions between care settings.
Features like abnormal-result alerts, standardized handoff workflows, and unified patient views are especially valuable in women’s health, where collaboration during pregnancy and postpartum care is common. More advanced systems can also use automation and intelligent routing to ensure the right information reaches the right provider at the right time.
Supporting complex billing and specialty workflows
Women’s health practices manage a wide range of visit types—from annual preventive exams to ultrasounds, prenatal labs, family-planning services, and delivery-related care. These services often extend over months and involve multiple clinicians, making documentation and billing more complex than in many other specialties.
EHR systems help manage this complexity by linking visits across episodes of care, improving charge capture, and supporting specialty-specific coding requirements. Automation reduces administrative burden, while structured workflows help ensure that services are accurately documented and billed.
Some EHR platforms include AI-enabled revenue cycle tools that streamline coding and reduce errors. Networked systems may also allow practices to benchmark performance against similar organizations, helping them align on best practices for coding and reimbursement. These capabilities support financial stability while allowing practices to focus on patient care.
Advancing research and understanding health disparities
Beyond individual care, EHR systems play an important role in advancing women’s health research. De-identified clinical data can be used to study trends such as maternal mental health, pregnancy-related complications, and long-term outcomes associated with reproductive health conditions.
As more women’s health practices adopt standardized data elements—for contraception, family planning, menopause care, and more—the potential for large-scale research continues to grow. Lifecycle-based care models also benefit from this data continuity, helping clinicians understand how earlier health events, such as gestational diabetes or preeclampsia, may influence future risks for chronic disease.
Enabling more connected, patient-centered care
From comprehensive documentation and coordinated care to efficient billing and research support, EHR systems are central to improving women’s healthcare at every stage of life. When paired with specialty-focused workflows, these platforms help clinicians deliver care that is not only more efficient, but also more connected and informed.
As women’s health needs continue to evolve, EHR systems will remain a key driver in creating seamless, data-driven, and patient-centered care journeys for women everywhere.




